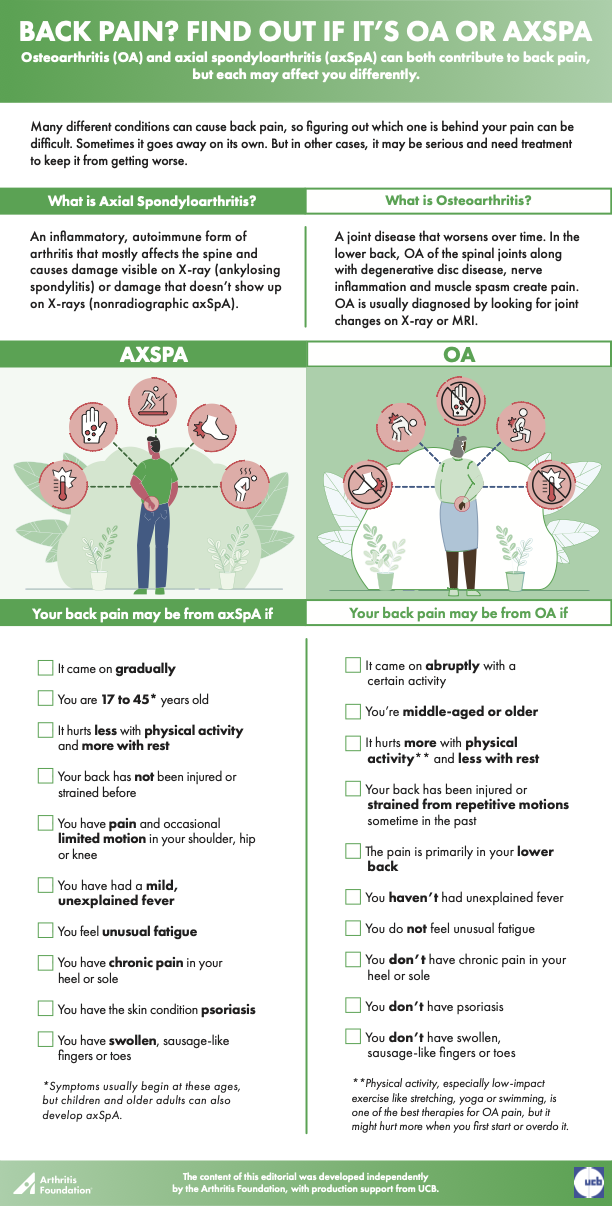
Back Pain? Find Out if It's OA or axSpA
Osteoarthritis (OA) and axial spondyloarthritis (axSpA) can both contribute to back pain, but each may affect you differently.
Sept. 14, 2022
Back pain is one of the most common complaints people take to doctors who specialize in arthritis. But figuring out why it hurts can be complicated because there are many causes of back pain. In some cases, it might clear up on its own. In other cases, it can be serious and require early treatment to keep it from getting worse.
Axial spondyloarthritis (axSpA) and osteoarthritis (OA) are two arthritis conditions that contribute to back pain.
OA is a disease of the joint that worsens over time. It can affect any joint, but when it occurs in the back, it affects the joints in the spine, called facet joints, and can contribute to pain. OA is more likely to affect lower back (lumbar) facet joints than the upper spine. In OA, the cartilage (a flexible tissue covering the ends of joints) can get damaged, and bony lumps (bone spurs) can develop around joints affected by OA. In the lower back, OA often combines with degenerative disc disease — changes to the “shock absorbing” discs between vertebrae — inflammation of nerve roots and/or muscle spasm to create mechanical low back pain. In most cases, OA is easily diagnosed by looking at changes to joints on X-ray or MRI.
AxSpA is an inflammatory, autoimmune form of arthritis, meaning the body’s immune system doesn’t work properly and attacks its own tissues. In axSpA, inflammation occurs where tendons connect to bone (called enthesitis) and where the spine connects with the hip joints, called the sacroiliac joints. Joint pain and swelling as well as fatigue are common axSpA symptoms, and inflammation may affect other parts of the body, as well. Other conditions may accompany axSpA, including psoriasis (affecting the skin, scalp and/or nails), the eye disease uveitis and inflammatory bowel disease (ulcerative colitis or Crohn’s disease).
There are two subsets of axSpA, which are distinguished by imaging used to diagnose them:
- In ankylosing spondylitis (AS), changes to the sacroiliac joints that are visible on plain X-ray.
- In nonradiographic axial spondyloarthritis (nr-axSpA), X-rays of the sacroiliac joints are normal or show only mild changes, but MRI images typically show changes. Some cases of nr-axSpA may progress to AS but not all.
Because axSpA — especially nr-axSpA — is not easily seen and its symptoms are similar to those of other diseases, it can be difficult to diagnose. In fact, it often takes years to get a correct diagnosis, which is why you need to understand how the signs and symptoms of axSpA differ from mechanical low back pain from OA or other conditions.
Click the image below to download the pdf file Back Pain? Find Out if It’s OA or axSpA
Here are some of the differences in symptoms and in those who are more likely to be affected:
Your back pain* may be from axSpA if
- It came on gradually
- You are between 17 and 45** years old
- You’ve had the pain longer than three months
- It’s worse when you get up in the morning or after you’ve been resting
- It gets better when you’re physically active
- It wakes you up at night after several hours of sleep
You may also have
- Fatigue
- Chronic pain in the heel (Achilles tendinitis) or sole of your foot (plantar fasciitis)
- Pain and occasionally limited ability to move other large joints, such as the shoulder, hip and knee.
- Psoriasis
- Swollen, sausage-like fingers or toes (dactylitis)
*A dull ache may initially be felt on one side or alternate. And symptoms vary among people, with pain beginning in other joints, such as the neck — especially for women — or the shoulder, elbow, hip, knee, ankle or heel.
**In most cases, symptoms begin at these ages, but they can also occur in children or older adults
Your back pain may be OA-related if
- It started acutely with a physical activity, like sports
- You’re middle-aged or older
- It hurts more with physical activity and gets better when you rest*
- Pain is worse at the end of a busy day
- Your back has been injured sometime in the past
- You’ve strained your back over time with repetitive motions — for instance, in work or sports
- You do not have fever, rash or unusual fatigue
*Physical activity is one of the best therapies for mechanical low back pain. In the early stages, it might hurt more, but keep at it. Start with low-impact exercises like stretching, yoga, tai chi, swimming or water aerobics. Strengthen your core muscles to help support weak joints. And be sure to use lumbar support to help maintain your posture and prevent further damage from twisting, bending, lifting or other potentially damaging activities.
Each condition is diagnosed and treated differently. Learn what to expect at your doctor visit.