Accumulator Adjustment Programs
Many arthritis patients use co-pay assistance, such as co-pay cards or manufacturer coupons, to pay for their life-saving medications. Pharmacy benefit managers (PBMs) and insurers increasingly use co-pay accumulator programs to prevent such assistance from counting towards patient cost-sharing, such as their deductible or annual out-of-pocket maximum. As a result, patients may struggle to afford and adhere to their medications as insurers and PBMs seek to shift more cost-sharing responsibility to patients.
The Issue
- Accumulator adjustment programs prevent any co-payment assistance that may be available for high-cost specialty drugs from counting toward a patient’s deductible or maximum out-of-pocket expenses.
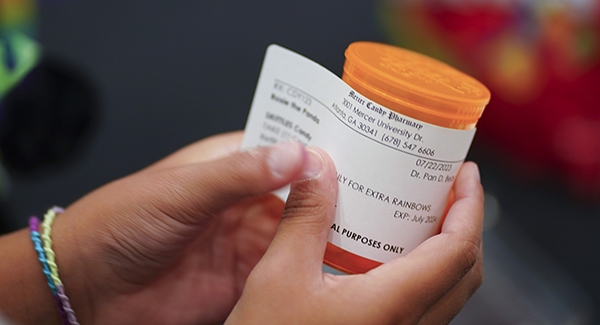
- Many pharmaceutical manufacturers offer co-pay cards that help cover a patient’s portion of drug costs. Traditionally, pharmacy benefit managers have allowed these co-pay card payments to count toward the deductible required by a patient’s health insurance plan. With an accumulator adjustment program, patients are still allowed to apply the co-pay card benefits to pay for their medications up to the full limit of the cards, but when that limit is met, the patient is required to pay their full deductible before cost-sharing protections kick in.
- Patients are often unaware they are enrolled in one of these programs until they go to the pharmacy counter and realize they must pay the full cost of their medication, which can lead them to abandon or delay their prescription. These programs can be called different names, are often marketed as a positive benefit, and are often disclosed many pages into plan materials, leading to a lack of awareness about them to patients.
- Example: It’s the start of a new health plan year in January and you are on a biologic with a list price of $3,000 a month. You use your co-pay card at the pharmacy and make a regular co-payment at the counter. By the time March arrives, you’ve reached the limit on your co-pay assistance. As a result, when you go to refill your prescription in April, you will owe $3,000, the full cost of your drug, because the deductible has not yet been paid down.
The Solution
- When calculating a patient’s overall contribution to any out-of-pocket maximum or any cost-sharing requirement, a health plan must include any amounts paid by the patient or paid on behalf of the patient by another person.
The Trends
- People most likely to be enrolled in co-pay accumulator adjustment programs include those with employer-sponsored insurance plans, particularly individuals enrolled in high-deductible health plans (HDHPs). HDHPs have become increasingly popular as employers and insurers seek opportunities to incentivize appropriate health care utilization and to lower costs.
- In an Arthritis Foundation survey of more than 600 patients, we found that:
- 41% of patients have a HDHP
- 84% said that a large, unexcepted charge for a prescription drug would impact their overall budget. When faced with that unexpected charge, 24% of patients said that they did not fill their prescription, and 8% of patients said they did not take their prescription as prescribed.
- 39% of patients on an employee-sponsored health plan used a drug manufacturer co-pay card to help pay for their arthritis medications. Among these individuals, 59% reported that they can use it to pay for their deductibles, 27% reported they can’t use it for their deductible and 14% reported that they don’t know.
- In a recent survey of employers, nearly 30% implemented a CAAP for 2019 and 21% were contemplating one for 2020 or 2021. In another recent employer survey, 54% of respondents did not credit third-party co-pay assistance toward patient deductibles.*
*Source: American Journal of Managed Care, Impact of a Co-pay Accumulator Adjustment Program on Specialty Drug Adherence
Our Work
- The All Co-pays Count Coalition (ACCC) was formed to provide a collaboration amongst the patient and provider community around legislative and patient education efforts on a federal and state level. The Arthritis Foundation sits on the steering committee for the ACCC and co-chairs the state subgroup.
- Specifically, the Arthritis Foundation has led and/or has been involved in efforts to educate legislative leadership in all 50 states as well as all 50 state insurance commissioners.
- On a state level, legislation has been enacted in Arizona, Arkansas, Colorado, Connecticut, Delaware, Georgia, Illinois, Kentucky, Louisiana, Maine, New Mexico, New York, North Carolina, Oklahoma, Tennessee, Texas, Virginia, Washington, and West Virginia, in addition to the District of Columbia and Puerto Rico. The legislation enacted in these states will serve as model language in future legislative sessions around the country.
- On a federal level, the Arthritis Foundation has worked alongside coalition partners to build support for the HELP Copays Act in Congress, which would ensure copay assistance counts towards patient cost-sharing.
- The Arthritis Foundation has also created and disseminated educational materials on this issue through our Your Coverage, Your Care toolkit, FAQs, blog posts, webinars, round tables and twitter chats; and has worked to raise broader awareness of the issue through the media, conducting interviews with media outlets such as Kaiser Health News.